Trusting injection drug users with IV antibiotics at home: It can work


BOSTON — Two mornings a week, Arthur Jackson clears space on half of his cream-colored sofa. He sets out a few rolls of tape and some gauze, then waits for a knock on his front door.
“This is Brenda’s desk,” Jackson said with a chuckle.
Brenda Mastricola is his visiting nurse. After she arrives at Jackson’s home in Boston, she joins him on the couch and starts by taking his blood pressure. Then she changes the bandages on Jackson’s right foot. His big toe was amputated at Brigham and Women’s Hospital in November. A bacterial infection, osteomyelitis, had destroyed the bone.
Jackson is still taking intravenous penicillin to stop the infection. He came home from the hospital wearing a small medication pump that delivers a steady dose of penicillin via a PICC line. PICC stands for a “peripherally inserted” or “percutaneous indwelling” central catheter, and it resembles a flexible IV tube, inserted into Jackson’s chest.
“This all looks good,” Mastricola said, after making sure the line was clean and in place. “You don’t need me.”
When patients need weeks or months of IV antibiotic treatment but otherwise don’t need to be hospitalized, the standard protocol is to discharge them with a PICC line and allow them to finish the medication at home. It saves money and is much more convenient for patients.
But this arrangement is almost never offered to patients with a history of addiction. The fear is that such patients might be tempted to use the PICC line as a fast and easy way to inject drugs like heroin, cocaine or methamphetamine.
Jackson, 69, was addicted to heroin for 40 years. Although he’s been sober for years, most U.S. hospitals would force patients like Jackson to stay in the hospital, sometimes for eight weeks or more. But Brigham and Women’s in Boston, along with a few others in the U.S., is challenging that protocol, allowing some patients with a history of addiction to go home.
Supporters of the change argue that doing so boosts the chances these patients will stay on their antibiotics and beat the infection.
A small team of Brigham doctors and nurses started planning this unusual option shortly after opening the Bridge Clinic, a walk-in health center in Boston for patients seeking treatment for a substance use disorder. Dr. Christin Price, one of the clinic’s directors, said virtually every patient who injects drugs develops some kind of infection. It’s difficult to avoid injecting bacteria into the bloodstream when using drugs in an alley or a public bathroom. The national opioid epidemic has led, in many cases, to a parallel increase in diseases related to injection drug use, such as HIV, hepatitis C and bacterial infections of the heart and bones. A study of North Carolina hospitals found a twelvefold increase in cases of bacterial endocarditis, a heart infection, from 2010 to 2015.
“Every time someone uses injection drugs, they’re putting themselves at risk for a very complicated infection,” Price said.
Treatment options for endocarditis patients with a history of drug use are limited. Some skilled nursing facilities, home care agencies and antibiotic infusion companies decline to work with these patients once they’re released from a hospital. And, Price said, some of her patients aren’t willing to remain in a hospital for weeks on end just to finish a round of IV antibiotics.
“They kind of get stir crazy,” she said. “You can imagine it’s almost like being held captive for six weeks, especially when you’re feeling fine now because the infection is clearing. A huge problem is that some of them can’t last — and so they leave before the six weeks are over.”
Patients who don’t complete their course of antibiotics can end up with a recurring infection and a repeat trip to the hospital.
Doctors and nurses affiliated with the Bridge Clinic wondered if there was a way to send patients with a history of drug use home — safely. They mapped out three requirements: First, patients would have to be taking an addiction treatment medication such as buprenorphine, or be willing to start one. Second, patients would have to check in weekly at the Bridge Clinic. Third, patients would need to have stable housing, and live with a sober friend or loved one. Price and colleagues began months of discussions with specialists in heart, bone and joint conditions, seeking buy-in from surgeons and nurses, so their patients could participate.
“A lot of people did sort of look aghast,” Price said. “It was just their policy that people with a history of injection drug use would not go home.”
When Dr. Daniel Solomon, who is also with Brigham and Women’s, encountered those looks, he said, he’d remind colleagues that “the alternatives aren’t that good either.”
Holding patients for weeks in a hospital room is hard on both the patients and medical providers, he said. And if patients want to use drugs, they’ll find a way to do it, even in a hospital bed.
In spring 2018, Price, Solomon and others enrolled a few of the first qualified patients, then a few more — intentionally cherry-picking those who wanted to be in treatment and had a sober, stable home.
Jackson met the requirement that at-home PICC line candidates take addiction treatment medication. He had been on methadone for 10 years, used heroin again, then switched to Suboxone, a combination medication containing buprenorphine and naloxone, which he has been taking for two years. And, in fact, Jackson said he was insulted when one of the doctors presented the home treatment option to him but said she was worried the PICC line might entice him to inject heroin.
“Stop right there,” Jackson recalled telling the nurse. “When it comes to my recovery, I’m serious because I’ve done so much to lick this — this thing.”
“First thing I thought was, ‘Oh, I could inject heroin in here easily,’” Jackson said. “But I dismissed that thought because I’m not going back” — back to winters on the streets and living from one heroin fix to the next.
“Everyone makes such a big deal about this PICC line,” said Stephen Connolly, 36, who went home with the open port last year, while being treated for endocarditis. “If I want to get high, I know how to do it. I’m not going to mess around with a PICC.”
Connolly said that when he first came to Brigham and Women’s Hospital he was focused on his heart, ignoring his other disease: addiction. He said he was surprised when every doctor he saw, even his cardiologist, wanted to talk about addiction.
“I’m like, ‘Listen, dude. My heart’s falling apart here, so let’s hold up with the drug talk,’” Connolly recalled. He assured the cardiologist he had his addiction under control, even though he wasn’t so sure. “Obviously, I didn’t, but my mind tells me that. It’s just crazy.”
Connolly said he realizes now that the conversation around drug use was relevant and related to his heart infection.
Connolly finished his antibiotic treatment while staying with family members in Abington, Massachusetts. Brigham doctors say the housing requirement excludes otherwise eligible patients. Recent research shows homeless patients who have HIV or hep C do take their antiviral medicines; there are no equivalent robust studies on treating homeless patients who have bacterial infections.
Nevertheless, a few other hospitals are testing ways to continue outpatient treatment for patients who don’t have a stable home. In Portland, Oregon, a medical center tried providing IV antibiotics inside addiction treatment programs. A hospital in Kentucky combines addiction treatment, counseling and outpatient IV antibiotics. In Vancouver, British Columbia, the Canadian national health program pays for small apartments, staffed with a nurse 24 hours a day, where patients can stay while they complete antibiotic treatment.
“People who use drugs deserve the same standard of care,” said Dr. Christy Sutherland, medical director at the Portland Hotel Society in Vancouver. “We can’t change what we offer as clinicians — to give people subpar treatment with the excuse that they are IV drug users.”
Jackson lives alone in his studio apartment (he does not live with a sober friend or loved one), but he convinced doctors he’d be better off there than in the hospital, so he could visit his 93-year-old mother daily, feed his tankful of tropical fish and his cat, and attend regular Narcotics Anonymous meetings.
Jackson is one of 40 patients with a history of drug use the Brigham team has discharged from the hospital to complete IV antibiotic treatment at home. The team is paying particular attention to 21 patients within that group who, unlike Jackson, are active drug users. So far, these men and women have finished their antibiotic treatment via a PICC line with no complications. One had to be readmitted because he had trouble administering the antibiotics. Price said three patients relapsed into drug use, but no one used the PICC line to inject illegal drugs.
“I think we’ve shown, through this pilot, that it is safe and feasible for certain patients,” Price said.
Taken as a group, the 21 high-risk patients who needed IV antibiotics spent 571 days at home rather than in a hospital or rehab facility. Not including the cost of home care visits by a home nurse, the savings tally more than $850,000, based on estimates of $1,500 per hospital day.
(Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation. This story is part of a partnership that includes WBUR, NPR and Kaiser Health News.)

Dr. Dareen Siri, an allergist/immunologist at Midwest Allergy Sinus Asthma, demonstrates how the PulmOne PFT Outside the Box works in her office in Normal. The desktop device allows the physician to make lung volume measurements without requiring a patient to climb into a pulmonary plethysmography cabinet that can cause anxiety in some patients.
DAVID PROEBER, THE PANTAGRAPH
Dr. Dareen Siri, an allergist/immunologist at Midwest Allergy Sinus Asthma, which has offices in Normal and Decatur, uses an anatomical model of the sinuses to explain why many people's heads feel like rocks during this spring's allergy season. She said the late winter delayed tree and grass blooms, forcing them to spread pollen all at once.
DAVID PROEBER, THE PANTAGRAPH

Dr. Dareen Siri, an immunologist at Midwest Allergy Sinus Asthma, demonstrates the use of an XHANCE inhaler for the treatment of nasal polyps. By blowing into the device, the throat naturally seals off from the nose and helps the medicine reach deep into nasal passages.
DAVID PROEBER, THE PANTAGRAPH
Dr. Dareen Siri, an immunologist at Midwest Allergy Sinus Asthma, sets up the PulmOne PFT Outside the Box in her office. The desktop device allows the physician to make lung volume measurements without requiring a patient to climb into a pulmonary plethysmography cabinet that can cause anxiety in some patients.
DAVID PROEBER, THE PANTAGRAPH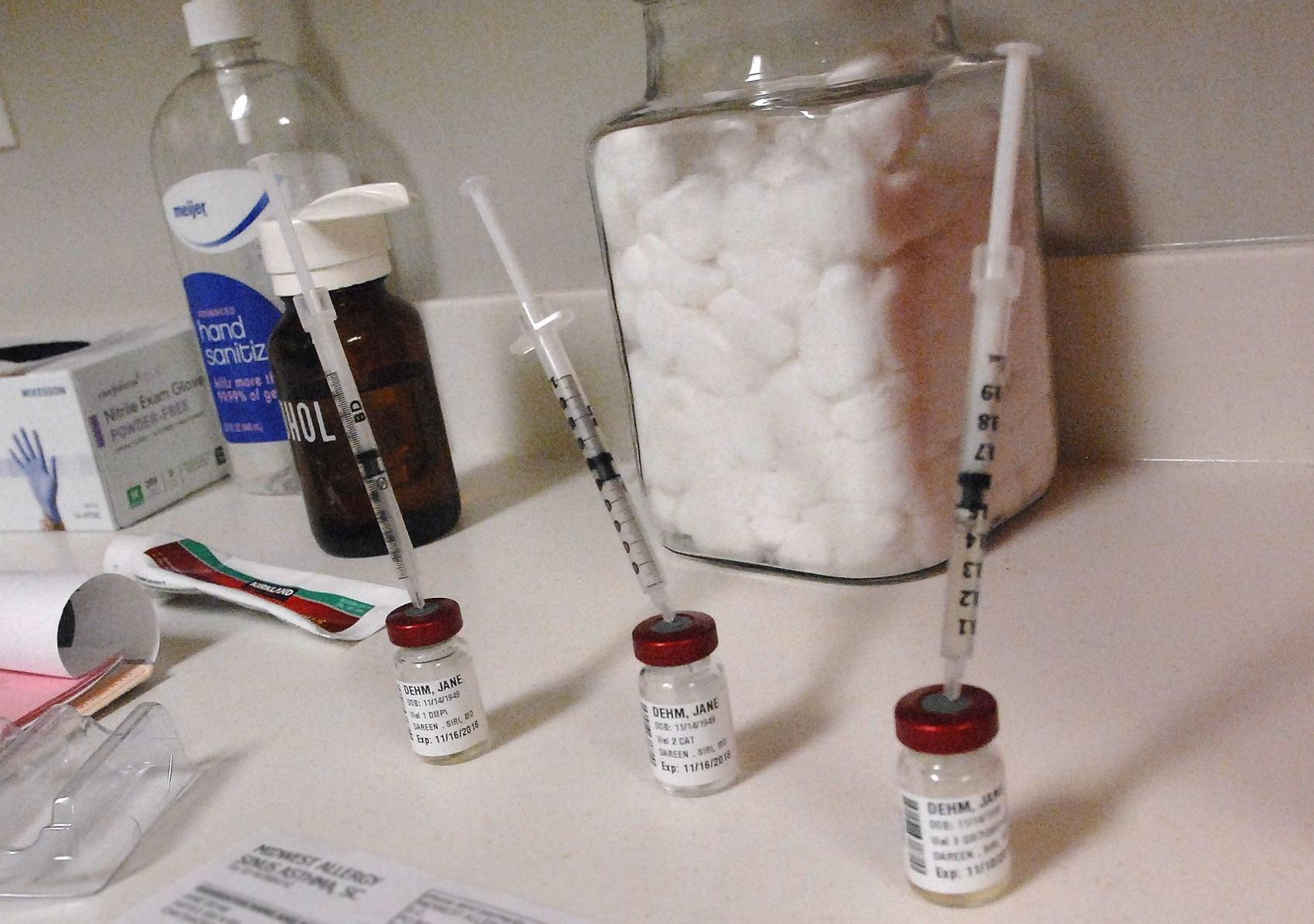
While some patients at Midwest Allergy Sinus Asthma, like Jane Dehm of Chatsworth, prefer the use of injectable allergy treatments, Dr. Dareen Siri is finding sublingual immunotherapy an option for some patients.
DAVID PROEBER, THE PANTAGRAPH

 Pathways Drug Rehabilitation Luxury Addiction Treatment & Detox Center
Pathways Drug Rehabilitation Luxury Addiction Treatment & Detox Center


